Exercise, Meditation & Yoga

So why exercise?
Scientific research has demonstrated significant benefits to exercising before, during, and after pregnancy!! Let’s look at the benefits for you and your baby!
Benefits –
- Less aches and pains
- More energy, less tiredness, better sleep
- Better adjustment to the physical changes in your body
- Reduction in varicose veins
- Reduction in swelling of the feet and ankles
- Improvement in muscle tone, strength and endurance
- Promotes a sense of wellbeing
- Reduces stress, anxiety and depression
- Improvement of medical conditions such as gestational diabetes (improves blood sugar levels) and high blood pressure (assists in lowering blood pressure)
- Reduces the risk of colon and breast cancer
- Women who do strength conditioning exercise also are more likely to have shorter delivery times and fewer complications
Risks to you while pregnant –
- Getting too hot due to dehydration or over-exertion especially during hot summer months
- Lower blood pressure causing you to feel faint when laying on your back usually after 16 weeks of pregnancy
- Physical injury due to looser joints caused by hormonal changes getting ready for birth
- Insufficient oxygen in the baby at high altitudes such as mountain climbing
- Lower blood sugar levels caused by not eating well during pregnancy
- Loss of balance caused by that growing baby
Types of Exercise:
There are two types of exercise we recommend during pregnancy –
- Aerobic exercise
- Strength conditioning
Aerobic (energetic) exercise is also known as cardiovascular exercise (heart and lungs). When you do aerobic exercise, your heart rate increases, causing the blood to circulate around your body and allowing oxygen to reach your muscles. Swimming, walking, running, aqua aerobics and dancing are examples of aerobic exercises.
Strength conditioning exercise helps to increase your overall fitness and involves slow controlled movements such as weight bearing exercises.
If you currently do not exercise routinely, we want you to begin with no more than 15 minutes continuous exercise three times per week for two weeks, gradually increasing to 45-minute sessions four times per week to daily.
If you currently exercise regularly before pregnancy, you should be able to engage in the same higher intensity exercise programs, such as running and aerobics, with no adverse effects for you or the baby. As your pregnancy progresses, you should be aiming to gradually reduce your overall activity and listen to your body. Stop an exercise when it starts to become uncomfortable that day. Continue with your routine changing exercises to suit “the belly” – crunches will obviously become more difficult with a growing baby, therefore, you may want to switch to something easier like leg raises.
We do not recommend any contact sports, such as kickboxing, martial arts, squash, volleyball, football, soccer, and ice hockey, due to the risk of being kicked or hit in the abdomen or falling directly on your abdominal area.
You should also be extremely cautious when doing exercises where there is a possibility of falling or losing your balance (horseback riding, skiing, gymnastics and cycling). In pregnancy, joints are less stable, your centre of gravity is altered as the bump overbalances you, and your reactions are slower.
Scuba diving is not recommended during your entire pregnancy, as your baby has no protection against decompression sickness and gas embolism under water.
Lastly we want you to avoid mountain hiking or climbing over 2500 metres until you have acclimatized and only with previous experience!
When should you stop exercising?
You should discontinue your exercise program if you have any unusual symptoms. If your symptoms began during aerobic exercise, it is important that you do not bring your exercises to an end abruptly as this can make you feel very faint. Instead, you should either walk around slowly for a short while or continue transferring your weight from one foot to the other by lifting one heel and then the other.
Unusual symptoms can include dizziness or feeling faint, headache, shortness of breath, difficulty catching your breath during exercise, weakness in your muscles, mild pain in your pubic area or abdomen. These symptoms can often be relieved with rest, a warm bath, a large glass of water, something sweet to eat if feeling faint and slowing down the pace of your exercises in the future.
We advise you to call your midwife for bleeding, leakage of your ‘waters’ (amniotic fluid), painful uterine contractions of preterm labour, fewer movements from baby following a kick count, or anything else that is concerning to you.
Can I train for athletic competitions?
If you are an athlete, you can continue to train for competitions. A healthy, low-risk pregnancy should not put you at risk of harming your baby in continuing to train throughout your pregnancy; however, we advise you speak to your midwife first to make sure you have proper supervision.
Hormonal changes mean your body will release more relaxin, making you more injury prone. Many athletes find they suddenly have an injury despite good form and technique. It is advisable to begin with lifting smaller weights to ensure your body is comfortable with pregnancy changes, and then to work up to your “normal” weight-baring exercises over a few weeks observing form and posture closely as your body adapts to pregnancy. During the third trimester, you may find that such weight-baring exercises become increasingly difficult to maintain, and lowering weights to ensure good form will help to prevent injuries.
It’s a good idea to talk with your trainer about your requirements for additional hydration and nutrition. If you are an elite athlete, you should not expect to retain peak fitness, so you should be prepared for a reduction in your performance during pregnancy.
Yoga & Pregnancy -
Yoga for everyone
When we become pregnant, our body releases three hormones;
1. Progesterone:
-Increases hypothalamus; causes fat storage
-Increases basal body temperature
-Increases amount of sodium excreted by kidneys
-Decreases gastrointestinal mobility
-Decreases smooth muscle tone of bladder, stomach, intestines, uterus, sphincters
2. Estrogen:
-Increases blood flow
-Growth and function of uterus and breast
-Sodium and water retentions
-May influence emotional mood swings
-Increases pliability of connective tissues
3. Relaxin:
-Relaxes the tendons, muscles and ligaments. This hormone facilitates the birth process by causing a softening and lengthening of the cervix and the pubic symphysis (the place where the pubic bones come together)
-Relaxin is released into the body immediately after conception and peaks at 3 months. It remains constant until labor where there is a significant rise.
You will notice with all three of these hormones, a common denominator is that in some manner or another, there is instability being created in the body by the softening of connective tissue, ligaments and tendons and smooth muscle tone. This, of course, is necessary to create the space for the growing baby, placenta and uterus. However, because of this “loosening” effect on the body, it is important to be mindful of one’s yoga practice, even early on.
Benefits of Yoga
Yoga offers so many benefits to you and your baby throughout your pregnancy and into the postpartum. Some of the reasons we love yoga so much include:
- Overall improvement of fitness
- Openness and strength to prepare your body for pregnancy and labour
- Breath awareness that can help during your labour
- Connection to your body and your growing baby
- Stress reduction through your practice and through meditation
- A reduction in water retention…aka less fat ankles!
- A reduction in lower back pain and sciatic pain
- A faster, more speedy recovery following birth
- Acceptance of your beautiful changing body
The First Trimester (first 12 weeks of pregnancy)
We recommend that in your first trimester, you begin to modify your yoga practice. It seems early; however, your body is going through tremendous hormonal surges. This stage of pregnancy is considered the most delicate because the risk of miscarriage is at it’s highest. Due to lack of evidence based research, some yoga instructors advise against doing specific poses to reduce the chance of miscarriage, and a systematic review and meta analysis in 2005, demonstrated hot yoga should be avoided in the first trimester (first 12 weeks of pregnancy) although not proven, could have an increased risk of neural tube defects and other anomalies to a fetus.
The Second and Third Trimester (13 weeks and beyond)
If you have not already taken up exercise in your pregnancy, and wish to do so, the second trimester is a great time to start with the approval of your midwife or doctor. We recommend a prenatal yoga class to anyone who is inexperienced or new to yoga provided they have a low risk healthy pregnancy. Should you be more experienced in your practice and/or practice yoga on a regular basis, we understand that you may want to continue with your previous practices modifying as your belly grows or recommencing your hot yoga practice, again modifying your practice based on how you feel. If you have experience with hot yoga, then you will already know how to adapt to this warmer environment. There are no studies to date with evidence suggesting hot yoga is unsafe during these stages of pregnancy. Clients living in hot climates do not discontinue exercising or taking hot baths. You may want to find a studio that will make you feel comfortable, and give you support to make sure you are following safe practice modifications. Some studios prefer to adapt their class to a pregnant practitioner in the room by lowering the temperature to just below 100 degrees in the heated room.
Recommended Modifications
Here are some suggestions for the more experienced practitioner:
Prone poses – Belly down poses can be continued, like bhujangasana (cobra pose), as long as you are grounding the pubic bone and elongating through the lower back, actively using your legs so the lower belly does not get any pressure. Danurasana (bow pose) and Salmbhasana (locust pose) should be avoided as they put direct pressure on the uterus.
Deep twists – These poses are an excellent means of compressing the internal organs, stimulating, and cleansing them. We recommend avoiding deep belly twists, but focus instead on twists of the upper back, keeping the belly facing forward and twisting above the bra strap line.
Deep backbends – These poses should be avoided as they stretch the abdominal muscles.
Jumps and Jerky movements – These poses should be avoided as they can disturb implantation.
Abdominal strengtheners – We recommend avoiding these during the first trimester and reintroduce transverse abdominal work in the second and third trimester. Doing abdominal exercises in pregnancy aids and prepares the client for the second stage of labour – PUSHING!! It also supports the back as the uterus continues to grow.
Pranayamas – You should avoid pranayamas that involve breath retention and deep forceful movements of the belly like kapalabhati or bhastrika (bellows breath). Alternate nostril breathing is fine as long as you do not add retention. Ujjiyi breath should also not be practiced. Since prenatal yoga aims to prepare you for labour, we encourage you to practice mouth breathing in your asana practice, so you become familiar with them during labour and birth.
Other good routines to practice
- Drink lots of water prior to and after your practice especially if you are practicing Bikram (heated) yoga.
- Bring a healthy snack for after class
- Find out where the cooler parts of a hot yoga studio room is and aim to lay your mat there
- Be guided by your comfort. If you have pain, stop. If you feel dizzy, lay down or leave the room. If you need to lean against a wall for balance, do so. If you need to urinate, do not wait!
- Give yourself 15 minutes of rest following class before you go home, especially following a hot yoga practice.
- At the end of class, Kapalabhati breathing is a great time to practice your pelvic floor exercises.
Local yoga studios will usually offer specialized and modified prenatal yoga programs as well as mom and baby yoga programs with certified instructors to guide you in your practice whether it be new or experienced.
Please note: Not all yoga studios support pregnant clients in their journey towards health through yoga practice. We encourage you to find a safe and supportive environment for your practice of yoga. Do not hesitate to ask a yoga studio for their policy regarding practicing while pregnant.
Pelvic Floor Exercises -
The pubococcygeal muscle otherwise known as the Kegel muscle, was named after the doctor who invented these exercises. We will call it the PC muscle for short. The PC muscle is like a hammock of muscle attached to the pubic bone and spine. It wraps itself around the vagina, urethra and rectum.
The hammock will hold all the inner organs up if it is strong enough.
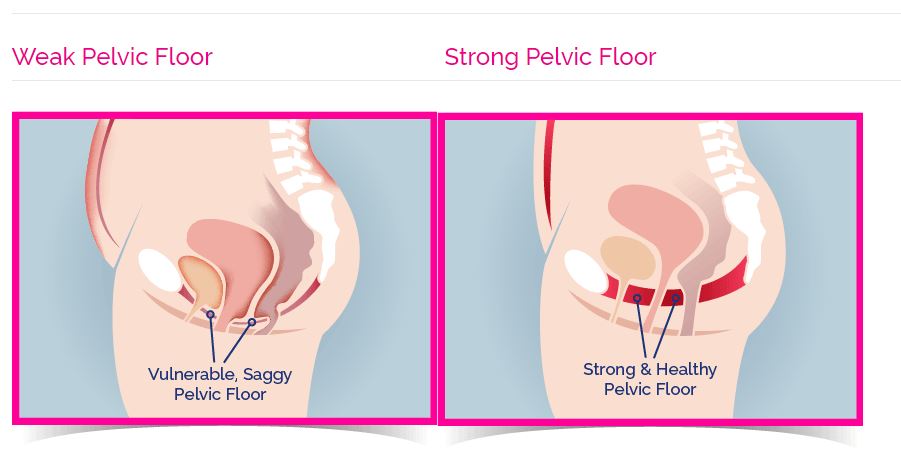
If it is weak, the bladder tends to sag, meaning every time you cough or sneeze, you leak urine. It also means your uterus is not high towards your belly button but also falls down into your vagina. This can even cause your uterus to begin protruding out of your vagina in some clients called uterine prolapse.
A weak pelvic floor can also affect sex, as it can cause reduced sexual sensation for both you and your partner. When the uterus sags, a shallow feeling can be felt inside the vagina, as if the penis or vibrator were thumping into something. This feeling is your cervix. This shallow feeling is a short, squashed, loose vaginal wall, meaning good penetration cannot be achieved, depriving both you and your partner a strong sensation during intercourse.
There are hardly any tactile nerve endings in the vagina. The kegel muscles are the “feel good” muscles during intercourse. So, this means, if the pelvic floor is strong and tight, a great deal more pleasure from deep-touch stimulation of the nerve endings.
Ok so how can we fix our saggy PC muscles:
STEP ONE:
The first simple exercise is to stop yourself from urinating the next time you feel the urge to urinate. With you legs apart, stop the flow of urine without putting your knees together. This doesn’t mean you have a strong muscle, but it helps you to figure out which muscle is the PC muscle.
STEP TWO:
Let’s practice by using 3 techniques –
1. Flex the PC muscle tightly by squeezing the muscle to prevent you from urinating, only do this when you’re sitting in a chair. If you are pinching your buttocks together then you are using the wrong set of muscles. A feeling of strain in the lower abdomen also means you’re doing them incorrectly. You should feel the muscles tightening first near your rectum (bum) and then continue to tighten towards your clitoris. After a little practice, you should be able to flex tightly, deeply and way up high. We want to do this around 300 times per day, which works out to 10 minutes with a few seconds rest between contracting your muscles.
2. Once you can flex your PC muscles and repeat it numerous times, you can discontinue your 300 flexes! Now we begin by flexing the muscles 36 times but hold it each time to the count of ten before releasing. Hold tightly and deeply. Do this 12 times in the morning, then 12 times in the afternoon, then 12 times before bed.
3. When you can hold the flex 36 times, we can move to an advanced conscious-release exercise. Flex just the outer third of the vaginal barrel, then the middle part, and finally up high. Release up high, release the middle third, then release the lower third of the vaginal barrel. Think of it like an elevator going up and down. Aim to do around 12 flexes a day to retain the tone you have gained, then do about 6 one, two, three release, two-three exercises.
4. Before the birth, try a couple of times to place your hand on your perineum, and as you are doing the release two, three exercise, try actively bulging your perineum outward as you release even more. The bulging down and releasing the muscle creates downward pressure for when you are pushing your baby out. Don’t practice this regularly, though!
Postpartum -
So now that you’ve had your beautiful baby…now what? Well, we encourage you to begin your Kegel exercises right after birth. PC exercises restore circulation as well as promoting healing and preventing uterine prolapse. Find a habit within your everyday activities to help you remember to do your exercises, whether it’s setting a reminder app on your phone or doing them every time you hit a red light driving to and from your destination!
Exercise after a vaginal birth:
Recovery following a vaginal birth can vary in length dependent on many factors such as whether you needed stitches, or an episiotomy, or whether you required an assisted birth using forceps or vacuum; it can also depend on your pelvic health prior to having your baby. We recommend taking it easy for the first six weeks and begin with short sessions of gentle walking after at least a few weeks of rest and only if you feel like you are ready. It can take six weeks or even longer to fully recover/heal after a vaginal delivery.
Before returning to “high intensity” exercise such as jogging/aerobics, you should be able to hold a kegel contraction for 10 seconds.
Exercise after a caesarean section:
Recovery following a caesarean section can be tough. Most clients find it takes over six weeks to begin to feel like they can mobilize more with gentle walking and moving around the house more freely. We expect you to rest and recover for the first six weeks, doing very little in the way of exercise. No heavy lifting of anything other than your baby, no sudden movements or household chores during this recovery time to avoid strain of the abdominal muscles. There is little research on exercise after a caesarean section, so we hope this assists you with “getting back to normal”.
Even though you haven’t “pushed” a baby out of the birth canal, the abdominal muscles have undergone a major surgery. Or maybe you had attempted a vaginal delivery too and had a failed forceps delivery and your baby was born by caesarean section. Your new body has an incision, bruising to your internal organs, ongoing baby weight, pelvic floor weakness if you were in labour, pushing for a long time or failed instrumental delivery, and lots of healing to do on the inside with muscles, tendons & nerves being damaged.
Healing time – the incision takes around six to eight weeks to heal if you have had no complications during the healing process such as infection, but it takes up to nine to twelve months or more to fully recover, and sometimes longer for sensations to return with clients complaining of ongoing numbness and tingling.
Where do you start after having your baby…
1. The first day after your caesarean section, we recommend a few exercises to begin.
-
- Start with some breathing exercises – bend your knees up and support either side of your tummy with your hands. Take a deep breath in, hold for a count of two. Sigh the air out through your mouth. Repeat this sequence 3 or 4 times. This may make you cough.
- To improve the circulation in your legs and help prevent any blood clots from forming, keep your legs straight and bend the feet up and down. Circle them at your ankle firmly and rapidly – at least 20 times every hour.
- Next you can try some abdominal exercises. Lie down with your knees up. Breathe in gently, and as you breathe out, gently draw in the lower part of your tummy. Let go. Do this 5 times, several times a day.
- You may experience some discomfort in your back following your surgery. When sitting up in your bed or chair make sure you have a pillow in the middle of your lower back to maintain the normal hollow at waist level and sit well back.
- To get in and out of bed, bend your knees up with your feet on the bed. Roll onto your side, keeping your knees together, allow your feet to drop over the side of the bed, and push yourself into a sitting position with your hands. Allow your legs to swing to the floor. To get back into bed, reverse the process.
2. Day two to four after your caesarean section, continue the exercise as outlined above and add the following exercises –
-
- Pelvic floor – commence these as soon as the urinary catheter is removed. Begin holding the pelvic floor contraction for 5 seconds and then release the muscle slowly, repeating the exercise regularly throughout the day. You can read about pelvic floor exercises above.
- Pelvic tilting/rocking – this will assist with “bowel gas”, backache and strengthening the abdominal muscles. Repeat five times. Gently tighten your lower tummy, while pressing your lower back into the bed gently. Pull your abdominal muscles in and up, hold for a few seconds then gently relax.
3. Day five after your caesarean section, begin stronger exercises for the abdomen.
-
- Knee rolling involves lying on your back, knees bent up. While pulling in your lower tummy and with your knees together, roll from side to side. Breathe normally. Repeat 5 times.
- Next, lay on your back with your knees bent. Tighten your lower abdomen and raise your head and shoulders. Slide your hand towards your knees, keeping the small of your back pressed into the bed. Repeat 5 times. Then try raising your head, but with your right hand reach out to touch your left thigh and then switch sides. Repeat 5 times on each side.
- These exercises should be done twice a day, 5 times each. Continue your exercises for at least 6 weeks, aiming to increase them by 1 a day until you are doing 20 of each exercise.
4. After two to six weeks, you can begin exercises like walking depending on how you feel – but don’t overdo it! Light household chores can begin around four to six weeks, but again, your body is healing and may need more time for rest so keep chores short to begin with. After six weeks, and only if you feel comfortable, start with low intensity cardio like a short bike ride of only 15 minutes and increase your workout duration by 5 minutes every two weeks. Workouts should be built up to 30-40 minutes in length aiming for three to four sessions per week. Strength training should consist of your bodyweight resistance only using resistance bands or very light weights. Examples include bodyweight squats, modified side planks, bodyweight split squats, band pull aparts and inverted rows.
Activities to avoid during this time are running, jumping, step ups, heavy weight training, crunches, leg raises, overhead press, front planks, and other traditional abdominal exercises as well as anything with downward pressure like barbell back squat.
5. After at least eight weeks following a caesarean section, low impact abdominal exercises can be commenced very slowly and very cautiously. Pelvic tilts and seated isometric abdominal squeezes will help to strengthen your abdominal muscles. Sit up tall and squeeze your belly into your spine. Start with 20 per day for the first four weeks and work your way up to 100. This should only be performed with no pain! More intense abdominal exercises should be avoided until the modified versions feel easy enough without pain to perform comfortably. If you had a vaginal delivery, be cautious with abdominal exercises stopping or modifying if you have an abdominal separation or feel any pain.
Other recommendations:
- We recommend obtaining a pelvic floor/abdominal wall physiotherapist specializing in postpartum care. They will not see you until six weeks postpartum. They generally do an internal and external assessment to design a recovery program specifically for your needs.
- Maintain good posture during your recovery time to ensure good healing alignment of the muscles and good circulation to the muscles for the healing process.
- Get back to your healthy diet and drink lots of water! This will greatly assist with post baby weight loss even if your exercise program only consists of short walks!
- Join a Stroller Bootcamp Group which assists specifically with postpartum weight loss, pelvic health and returning to a healthy fitness level. We do not recommend starting a bootcamp following a caesarean section for at least 3 months and only if you feel ready. Most experienced instructors/personal trainers will give you options to modify exercises appropriately.
- We advise you wait to go back to swimming until after your six-week midwife check.
