Labour
Early labour
Early labour is otherwise known as the latent phase of labour, when your body is in the beginning stages of “going into labour”.
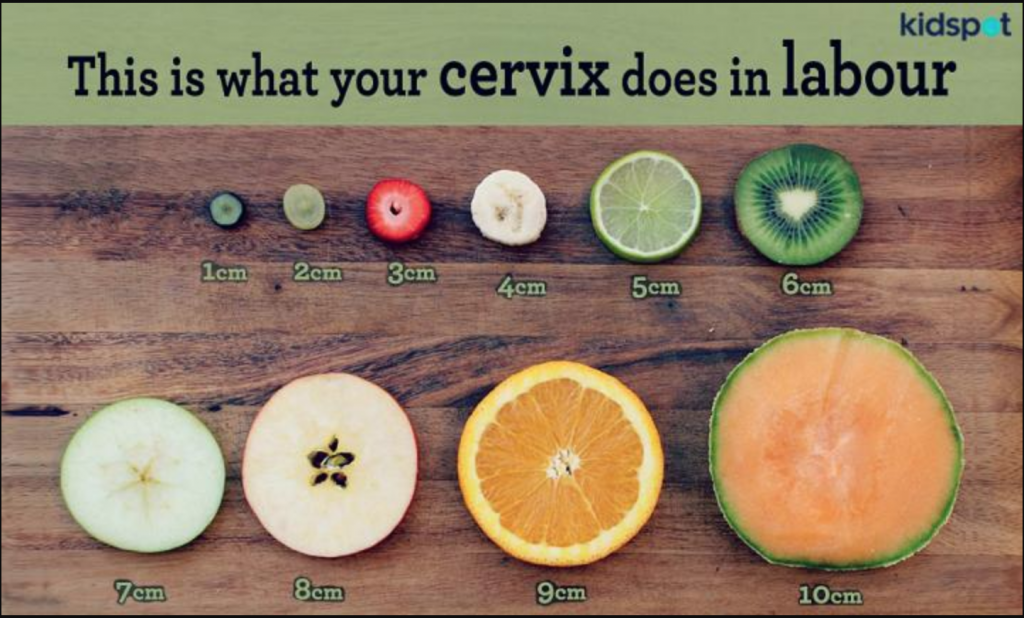
During pregnancy, your cervix will start off long, thick and closed (like in picture 1 of figure 1). When you get closer to the end of your pregnancy (or unless you go into preterm labour), your body will begin to make changes to your cervix by sending signals to your brain, to produce the hormone oxytocin which causes your uterus to have contractions, dilate your cervix and allow your cervix to thin out known as effacement. Your baby can then start to descend down the birth canal.
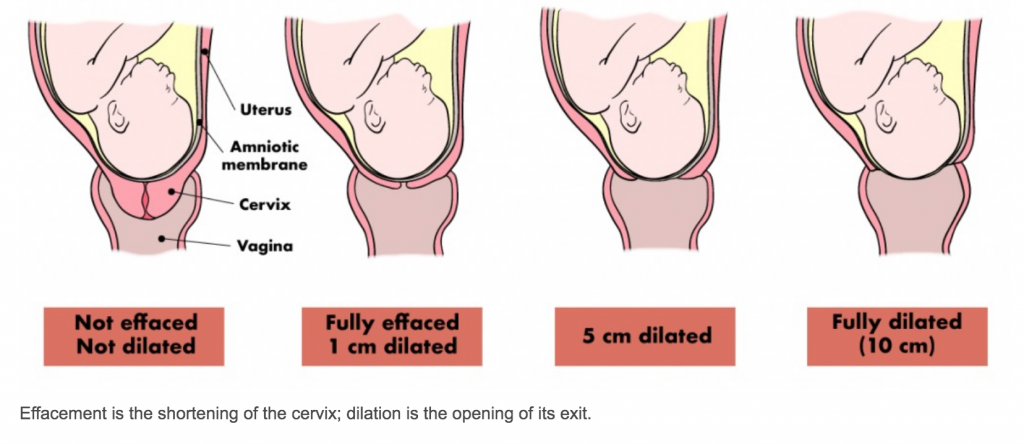

Active labour is around picture 3, figure 1. You will be 4-8cm dilated with a very thin effaced cervix. Contractions will be 3-5 minutes apart and lasting 60 seconds or longer. You will transition from 8cm to fully dilated then begin the “second stage” of your labour – pushing (picture 4, figure 1).
Signs of early labour:
There are many signs that you may be in early labour, however early labour can take a LONG time as your body needs to make many changes. We cannot predict how long this process will take as every person makes changes differently. This is very normal.
If it is your first baby, on average most people will experience around 8-12 hours of early labour contractions and/or tightenings. Sometimes early labour can also take a few days or sometimes even up to a week on and off before they become established, and by no means is early labour easy. Sometimes contractions can be strong, hard and painful for hours. This is normal.
Subsequent pregnancies usually have a shorter early stage of labour, but it is not uncommon for this stage to progress slower than you may expect. You may in addition have false labour where the contractions come strong, regular and close together (but never get much stronger) then disappear after an hour or two. This can be on and off for a few weeks prior to active labour. This is also normal.
Every pregnancy is different, but most people will experience one or more of the following when they are in early labour:
- Contractions that are irregular, lasting less than 60 seconds long, over a period of time. Most of these contractions are bare-able, some not so much. Most clients can talk through these contractions (even if they don’t want to).
- “Show”: thick mucous mixed with blood from the cervix. This sign can happen a few weeks before anything else happens, so we tend not to get too excited about this sign.
- Your waters might break. Note; the colour should be clear fluid, it should not have a foul odour, and your baby should continue to move. You should inform your midwife immediately if your water is green, yellow (but not urine) or black, your baby is not moving or the water smells foul. You should call your midwife if you are group B strep positive so they can discuss the next steps.
My contractions have started. Now what?
Contractions will often start as cramping in your lower abdomen, and/or lower back and gradually become stronger and more painful. They will be irregular, less than 60 seconds long over an unknown period of time.
Most people can talk or text through contractions at this stage – even if they don’t want to. Some contractions will be stronger than others. Some contractions will require you to focus and use breathing techniques to assist you with managing the contraction strength. This is also very normal during the early stages of labour. Your body has a lot of work to get done before you are in active labour.
Early labour instructions:
During these early stages, we encourage you to rest as much as possible and avoid timing contractions. It is important that you relax to allow your body to make the necessary changes to get you ready for active labour. Early labour however can be very painful, therefore we encourage you to take:
- Tylenol (Acetaminophen) 1000mg orally every 4 hours (Max 4000mg in 24 hours)
- AND Gravol (Dimenhydrinate) 100mg orally every 4-6 hours (Max 400mg in 24 hours) or a Gravol suppository if you are vomiting.
- Take a bath (preferred) or shower. In fact take several, this will help your pelvis relax and provide natural pain relief,
- Take gravol and have a nap – even if you are unable to sleep, the medication will allow you to be drowsy enough to close your eyes between contractions,
- Put your TENS machine on if you have one,
- Take your mind off the contractions between resting by watching a movie, reading a book, going for a walk, baking a cake, doing any activity where you can keep busy.
- Have a good meal and lots of snacks between contractions, and stay hydrated.
- Have your birth partner give you a back massage or squeeze your hips during contractions.
- Use a heat pad for natural pain relief.
- Use gravity – stand up, lean over, hula hoop your hips, sway from side to side, dance to music, lunge with one foot on a step or use your stairs.
Should I call my midwife in early labour?
It is not necessary to call your midwife when you are in early labour. We prefer to know once you are in active labour so that in the meantime we can get lots of rest so that we are ready to assist you in labour. By calling your midwife early, she may be sleeping at the time and unable to get back to sleep after your call, or dealing with another client in labour. As exciting as this moment is, there is not a lot of extra advise we can offer, other than following our early labour instructions, and ensuring you are getting lots of rest too since this process can take a long time.
You should call your midwife at any time in early labour if:
- your waters break and the fluid is green, black or a yellow colour (but not urine), or it smells foul as this can be a sign of meconium or infection,
- your baby is not moving or movements are decreased,
- you develop a fever or chills – temperature over 38°C (100°F).
- your baby is under 37 weeks gestation,
- you experience frank red vaginal bleeding.
- you have symptoms or someone in your household has symptoms of COVID-19
Active Labour
Active labour is when your cervix is 4-8cm dilated with a thin fully effaced cervix AND your contractions are regular, strong and long.
If you are a first time parent, you can follow the 3-2-1 rule = consistent contractions every 3-5 minutes, for 2 hours, lasting 1 minute or more.
If this is a subsequent pregnancy, you can follow the 5-1-1 rule = consistent contractions every 5 minutes or less, for 1 hour, lasting 1 minute.
If you have had a previous quick birth, you should use your judgement and call earlier if you think your contractions are strong and you need to breathe through them, even if it has not been long since they started or they are coming less than 10 minutes apart.

Have my waters broken?
If your waters have broken, you will experience a large gush of fluid coming out of your vagina or a constant trickle of fluid leaking enough to wear a sanitary pad. Your waters should be clear in colour, with no foul smell, and your baby should continue to move. You may already be having contractions, which may become more intense once your waters have broken. You may not have any contractions at all.
If you are “unsure” your waters have broken, we advise you to walk around without pants or a pad in place to see if fluid leaks down your legs. You can also lay on a couch or bed for five minutes then stand up without pants on. If your waters have broken, fluid will leak or gush down your legs. If you do not notice fluid leaking after the initial “gush or trickle”, this could indicate watery discharge or urinary incontinence, both of which are normal in the third stage of pregnancy. You should continue to monitor by wearing a pad, and if the pad is soaked within the next hour, you should call your midwife. If it is dry, then it is likely your waters have not yet broken.
You should call your midwife at any time if:
- you are in active labour,
- you are group B strep positive,
- your fluid is green, black or a yellow colour (but not urine), or it smells foul,
- your baby is not moving or movements are decreased,
- you develop a fever or chills – temperature over 38°C (100°F).
- your baby is under 37 weeks gestation,
- you experience frank red vaginal bleeding,
- you or someone in your household has COVID-19 symptoms.
My waters have definitely broken but i have no contractions. Now what?
Pre-labour rupture of membranes (PROM) is when your waters have broken but labour has not become established – in other words, you do not have regular painful contractions yet. It is normal and common in a term pregnancy. Around 10% of all pregnancies will experience PROM.
There are two options when this happens: the first is to wait for labour to start naturally (expectant management); or secondly is for induction of labour so that baby is born as soon as possible.
Expectant management:
Expectant management is offered to all clients who have had uncomplicated pregnancies, are group B strep negative (or unknown if you have decided not to test), are over 37 weeks gestation, your baby is head down and engaged in the pelvis, and your fluid is clear and odourless.
The Term PROM study, is the largest randomized controlled trial to date focusing on the management of PROM. Researchers recruited 72 hospitals in 6 countries (Canada, UK, Austria, Sweden, Demark and Israel) following 5041 pregnant people. This study wanted to compare the risks of waiting to go into labour naturally versus inducing labour after PROM, and see if one method was superior to the other. They concluded that expectant management versus induction of labour were both reasonable options after PROM and neither were superior to one another.
If we use the Term PROM study results, we can analyze the risks and benefits of waiting to go into labour by yourself including;
- Infection in the waters (known as chorioamnionitis); 8.6% expectant management vs 4% induction of labour. However, the higher rate could have been due to unknown GBS screening and multiple vaginal examinations during the study (which your midwife will avoid until active labour). Similar smaller studies who limited vaginal exams found a very small difference in these results compared to the Term PROM trial.

- Postpartum Fever; 3.6% expectant management vs 1.9% induction of labour.
- Caesarean section rate; 9.7% expectant management vs 10.1% induction of labour.
- Neonatal infection; 2.8% expectant management vs 2% induction of labour.
- 77-78.8% pregnant clients in the expectant management group went into spontaneous labour.
- Continuous electronic fetal monitoring and epidural use was higher in the induction of labour group compared to the expectant management group.
I am GBS positive and prefer expectant management:
In 2019, 9.6% of pregnant people in Ontario who experienced PROM were GBS positive.
The Term PROM study is the only study to date that also analyzed the risks of group B strep (GBS) positive clients wishing to choose expectant management over active management (“immediate induction of labour”). Of 5041 clients, only 4834 clients were tested for GBS at delivery. Researchers found a non-significant trend suggesting clients positive for GBS were at a lower risk for GBS disease of the baby if they were induced vs expectant management. However these results are skewed as many of the clients were unaware of their GBS status until after having their baby, which also meant that many clients were not treated with IV antibiotics during their labour. This contributed to the higher neonatal infection rates as seen above. The term PROM study does not provide sufficient evidence to compare the strategy of induction immediately with induction of labour after a moderate waiting period or with ongoing expectant management.
In 1999, the clinical practice guidelines (CPG) reanalyzed previously published data, which showed there was an increased risk of GBS infection to the baby the longer a client waited, but the risk was not statistically significant until 18 hours after the waters had broken. The study was also done prior to clients being screened for GBS or treated with IV antibiotics in labour. So it is difficult to determine whether these results are valid today.
The Association of Ontario Midwives recommends all clients are offered a choice between immediate induction of labour with oxytocin and expectant management when they are GBS positive due to research gaps in the most effective approach at preventing early onset GBS disease of baby.

They also recommend this choice less than 18 hours after rupture of membranes with no other risk factors present. Commencement of IV (intravenous) antibiotics via a drip in labour will be offered to all clients upon induction of labour or if spontaneously labouring if planning expectant management up to 18 hours. This requires a small needle to be placed in your hand or arm where a tube will be left in place throughout your labour with tubing attached to give you antibiotics and/or other fluids. This can be done at home if planning a home birth.
Vaginal examinations are avoided for all clients who experience PROM due to the known increase risk of infection.
When to call the midwife if choosing expectant management:
If you are planning to await labour, you should call your midwife once your waters have broken during the daytime so that she can make a plan to assess you and your baby.
If it is overnight when your waters break, AND your baby is moving, AND the fluid is clear, you can put a sanitary pad on, take 1000mg of Tylenol to help with the onset of cramping, and 100mg of Gravol to help you rest. You should call your midwife first thing the next morning.
If it is overnight when your waters break, AND you have abnormal signs as listed above (see “Have my waters broken?“), you should page your midwife immediately.
You should call again once you are in active labour so that your midwife can meet you for an assessment at home or the hospital.
Waiting for labour to start:
- You should take your temperature during waking hours every four hours, and call your midwife if you have a fever.
- Observe the water for colour change and smelly odour.
- Monitor your baby’s movements.
- Drink plenty of fluids.
- If you experience cramping or early labour contractions, try taking a bath or shower, take Tylenol (1 gram), use heat pads, apply your TENS machine if you plan to use one. You may take 1000mg Tylenol (acetaminophen) orally every 4 hours (Max 4000mg in 24 hours).
- Get lots of rest. You may take a medication to assist you with sleeping or helping you to relax between contractions. You can take Gravol (Dimenhydrinate) 100mg orally every 4-6 hours (Max 400mg in 24 hours) or a Gravol suppository if you are vomiting. An alternative medication to help you sleep, is Benadryl (Diphenhydramine) 50mg orally every 4-6 hours (Max 200mg in 24 hours). You may take Benadryl instead of Gravol, if Gravol is not working for you or you are unable to take Gravol due to an allergy.
- You can discuss other methods to naturally induce labour with your midwife such as castor oil, homeopathics, nipple stimulation and using the breast pump.
Induction of labour:
Induction of labour is offered to all clients immediately who are group B strep positive, have other risk factors for labour, fluid contains meconium (baby’s poop) – green or black poop coloured fluid will be leaking, or the client has a fever or other signs of infection. You should contact your midwife via the pager line to discuss the next steps.
If you are GBS positive, and have decided to choose expectant management, you may follow the steps above for calling your midwife.
If you have decided to choose the expectant management option, but nothing has happened and you are not in labour after a length of time, your midwife will discuss the best time to meet at the hospital to induce labour.
When baby arrives before midwife
If labour appears to be progressing very quickly (ie: you are feeling the need to push and the midwife is not yet present), please follow these instructions:
- Tell your partner to lay down on the bed – tell them not to walk around or sit on the toilet
- Call 911 and tell the dispatcher that your partner is in the process of giving birth
- Tell your partner to pant or blow when they have the urge to push
- If there seems to be time, warm some towels in the dryer or oven; these are to wrap the baby in. Otherwise, have some towels available where the baby will be born
- Try to stay with your partner and reassure them until help (either the midwife or the ambulance) arrives
- If there are children or others present who can assist, try to call for their help, if possible
- Have the phone close to you, if possible
- If the baby’s head is beginning to emerge, encourage your partner not to push so that the baby is born slowly to prevent tearing of the perineum
- Place the baby on your partner’s abdomen with its head down over your partner’s side so that mucous will drain out
- Wipe the baby off thoroughly and cover with warmed towels. It is VERY important that the baby is kept warm and dry
- Leave the cord attached to the baby – do not attempt to clamp or cut it
- If the placenta delivers, just leave it attached to the cord
- Do not worry about cleaning up – stay with your partner and keep them warm and reassured
- Put baby to breast, if possible
- REMAIN CALM – HELP IS ON THE WAY
