The Postpartum Period
You did it!!! You've just had a baby, so what now?
Congratulations from all of us at Thames Valley Midwives on your beautiful new bundle(s)!! We want to ensure you have a smooth transition to parenthood whether it’s your first baby, second baby, third baby, or more!
Birthing a baby sure isn’t easy and we know you must be exhausted, regardless of whether you were able to deliver vaginally, needed assistance with forceps or vacuum, or needed a caesarean section. We have a few reminders and a general “what to expect in the first week” discussions on this page, to jog your sleep deprived brain, when you can’t quite remember what the midwife told you! Let’s get started!



Right after the birth -
Delayed cord clamping:
Your midwife or OB team will perform delayed cord clamping for the recommended 60 seconds after your baby is born, in accordance with Canadian neonatal resuscitation guidelines, providing your baby does not require resuscitation.
Research has shown there are two main benefits associated with allowing the cord to remain attached for 60 seconds after your baby is born:
- Reducing iron deficiency as delayed cord clamping allows extra red blood cells to transfer from the placenta to your baby, increasing your baby’s blood volume by up to a third and improving stores in the first several months of life. Iron in the blood is vital for healthy brain development.
- Significant neonatal benefits in preterm infants. Decreased need to use medications to support baby’s blood pressure, better establishment of red blood cell volume, decreased need for blood transfusions, lower incidence of necrotizing enterocolitis and brain hemorrhage and possibly improved survival.

There is a small increase in the incidence of jaundice that requires phototherapy in term infants undergoing delayed umbilical cord clamping.
For clients having their baby by caesarean section at LHSC, delayed cord clamping will be performed immediately following delivery, before baby is placed in the nearby cot for your midwife or taken to the resuscitation area for further assistance.
Skin-to-skin contact:

There are many benefits of skin-to-skin contact right after birth and in the weeks following your baby’s arrival. Skin-to-skin is the practice of having your baby naked next to your own skin underneath clothing with a blanket covering you both.
We encourage skin-to-skin contact immediately after birth with you and/or your birth partner, or surrogate parents, to assist with stabilizing your baby’s temperature, heart rate and blood sugars. It also allows your baby to be colonized with your natural bacteria, as well as calms your baby if you plan to breast or chest feed. Baby’s will naturally start to root for the nipple when they are placed skin-to-skin prior to breastfeeding.
TIP – If you are finding your baby is very sleepy but due for a feed or you are having difficulty latching baby to the breast, put your baby skin-to-skin and allow baby to root for the nipple.
We encourage skin-to-skin contact for at least the first two hours after your baby is born, with a short break to allow your midwife to perform essential newborn care and allow you to eat, shower if you are able, and have your bed changed to make you both more comfortable. If your baby requires assistance from the neonatal unit team after birth, skin-to-skin contact will be established as soon as your baby is well enough. Your midwives will discuss skin-to-skin with the obstetric team should your birth result in a caesarean section.
If your baby is born prematurely, the neonatal unit team will assist you with skin-to-skin also known as “kangaroo care”, as soon as your baby is stable.
Your placenta:

Your placenta is the most remarkable organ that kept your baby fed and oxygenated throughout your pregnancy as well as removing any waste items and carbon dioxide out of your baby’s growing environment in utero.
However, after your baby is born, it also needs to be “born”!
We often tell parents that placenta’s do not have any “bones” so it is less painful coming out than when you pushed your baby out. Often clients will describe the feeling as “a lot of pressure”.
In some circumstances, we give an injection called oxytocin, to help deliver your placenta, or if we think you are bleeding too much after your baby is born, or if you have risk factors for bleeding prior to birth. This is called “active management”.
Once the placenta comes out, we check to make sure it appears complete and then it is disposed of in the hospital waste if you deliver at LHSC or WGH. You can request to take the placenta home if you wish to bury it or have your placenta encapsulated by a professional. For a home delivery, you will freeze your placenta until garbage day, and put it out in the morning, another alternative is to dig a very deep hole and bury it. Some clients will plant a tree.
You may also notice that we do frequent “belly rubs” in the first few hours, where we will massage your uterus just below your belly button to help your uterus contract and expel any unwanted clots. This can be uncomfortable for clients, so we want you to be prepared. We are not trying to hurt you, but this technique helps your midwives to stop you from bleeding significantly and ensures your uterus is contracting back down to pre-pregnancy size.
What else to expect:
Your midwives will continue to monitor your vital signs, commence an enormous amount of hospital paperwork (a lot less if you are at home), check your baby over thoroughly and monitor baby’s vital signs, administer medications as necessary, check your bleeding frequently (which means rubbing your belly frequently), help you to shower if you are mobile, assist with breast or bottle feeding, and clean up from the birth. If your birth has been straightforward, you should expect that your midwives will leave after a few hours. You may be offered a direct discharge home if you gave birth in the hospital, but your midwives will discuss the best course of care with you.
The initial newborn exam:
Your midwives will do a newborn examination around an hour after the birth to make sure your baby has all the necessary parts! We generally do a head-to-toe check looking for issues like tongue ties, hip dislocations, heart murmurs, birth marks, birth defects, bruising, and anything else we might come across. We will discuss any normal, unusual or abnormal findings with you and make any necessary referrals. We will weigh your baby, measure length and head circumference, and offer medications at this time.
We repeat this head-to-toe examination around 24 hours of age to ensure something hasn’t appeared a little later on.
Please note: we do not bath your baby(s) after they are born. It is important that your baby is kept skin to skin in the first 24-48 hours before attempting a bath so that baby can regularize their temperature and allow any of the white vernix moisturizer to soak into the skin helping with baby’s immune system.

Baby medications:
There are two common medications offered to give to your baby after birth.
- Vitamin K – given to prevent hemorrhagic disease of the newborn (HDNB). In a nutshell, HDNB presents with unexpected bleeding often occurring in the stomach and brain, which can lead to death. It is caused by a deficiency in vitamin K in the baby. If you wish to protect your baby against HDNB, we will give your baby the vitamin K injection during the initial newborn examination. There are no known side effects from the injectable form of vitamin K. There is an oral form of vitamin K repeated in three doses at specific times, which can be obtained from the States, however studies have shown that oral doses of vitamin K are significantly less effective than injectable and may be associated with higher incidence of failure.
- Erythromycin eye ointment – the use of silver nitrate eye prophylaxis became a mandatory procedure in the 1800’s to reduce the incidence of blindness as a complication of ophthalmia infection, caused by passing on gonorrhoea and/or chlamydia to the baby at birth. Today newborn ocular acquired gonorrhoea or chlamydia is rare, as we now know how to screen and treat people who have acquired these sexually transmitted diseases. However, prophylaxis remains a mandatory public health law in Ontario. Midwives are committed to providing evidence-based care to their clients. During the course of your prenatal care, your midwives will offer you testing to screen for gonnorrhea and chlamydia. Contrary to current public health policy, research evidence does not support mandatory neonatal eye prophylaxis as the agents used for eye prophylaxis show high rates of ineffectiveness. For this reason, most countries around the world have abandoned mandatory eye prophylaxis.
Other tests offered:
Your midwives will discuss and offer other tests for your baby including the following:
- Newborn Screening (NBS) – this test requires taking a small sample of blood by using a small needle to prick your baby’s heel after 24 hours of birth. The blood test screens for 28 different metabolic, endocrine, haematologic and respiratory diseases such as congenital hypothyroidism, sickle cell disease, cystic fibrosis, phenylketonuria, maple syrup urine disease (yes you heard that right!) Click here for a detailed list of diseases. The goal of screening, is to diagnose your baby and start treatment as early as possible. If your midwives performed your baby’s test, they will receive negative test results within around 3-4 weeks. Positive results are usually reported within a few days to a few weeks. If the test is positive, we will refer your baby to the right specialist for further testing. If your baby’s test was performed in the hospital, a paediatrician will receive any positive results and call you to organize a further referral.

- Critical Congenital Heart Disease Screening (CCHD) – this test is a quick non-invasive pulse oximetry test performed after 24 hours of birth. 3 in 1000 babies in Ontario will have critical congenital heart disease. A small light probe is wrapped around your baby’s hand and foot to measure the level of oxygen in your baby’s blood. This test is looking for conditions where a baby’s heart or major blood vessels around the heart are not formed properly. Often a baby with a critical heart condition will require surgery or intervention within the first year after birth. If your baby screens positive, the test will be repeated. If your baby fails the second test and you are at home, your midwife will send you on the same day to LHSC hospital’s children’s emergency department to meet with a specialist. Early detection has proven to have better outcomes when treatment is started early.

- Transcutaneous bilirubin measurement for jaundice (TcB) – Bilirubin contains a pigment that makes your baby’s skin look yellow known as jaundice. It takes a few days for a baby’s liver to become better at removing bilirubin from the baby’s blood. Most babies become jaundiced in the first week of life, but around 2% develop too much jaundice. TcB is a screening test that is performed anytime after 12 hours of age. It is a small non-invasive light test performed by placing a probe on your baby’s forehead or earlobe to check the levels of bilirubin in your baby’s body. Your midwife will also visually observe your baby for “too much” jaundice or recheck using this tool if it is felt your baby is at a higher risk of developing “too much” jaundice. If your midwife suspects too much jaundice or the TcB is abnormal, a serum bilirubin blood test (TSB) will be performed after a detailed discussion about the findings and overall clinical picture. If your baby’s TSB is abnormal, your baby will be placed in an incubator under special blue lights for treatment called phototherapy, which helps to break down the bilirubin faster. You can read more on jaundice below.

- Hearing screening – This screening helps detect 3 in 1000 babies born each year deaf or partially deaf. An earlier diagnosis can help to improve a child’s speech, behavioural and emotional development as they grow by providing help early on. Children with hearing loss can learn speech and language differently to prevent further delays in learning to talk. Once your baby is born, you will be offered a hearing screen after 24 hours if you deliver your baby at the hospital. If you give birth at home or leave the hospital before 24 hours or on the weekend, your baby will be referred to the Ontario Newborn Hearing Screen program. You will be contacted by the program with an appointment time and location within the next month after your baby’s birth.

The first week after birth -
Your midwife will visit you at home or at the hospital for the first week usually on day one, two or three, and four to seven postpartum.
We expect you to be resting for the first week and therefore our postpartum visits are not scheduled. Your midwife will come to visit anytime on the day arranged, sometimes this is early morning and sometimes later in the evening. If your midwife is sleeping from a birth, another midwife will be organized to visit you.
Please do not page the on-call midwife about your home visits in case she is at a birth or sleeping. If it’s more convenient for you to come to the clinic for your early postpartum visits, this can be arranged instead of home postpartum visits.
Please ensure during the winter months your driveway is shovelled and gritted for the safety of our midwives. During times of a snowstorm or unsafe driving conditions, your midwife will contact you to make other arrangements.
All pets should be caged, or placed in another room during your midwife’s home visits. Due to health & safety as well as allergies and fear of animals, our midwives and their equipment cannot come into contact with your pets.
During the initial weeks after you have your baby you can refer to this online guide, our resources page as well as watching the educational videos in our postpartum section to assist you with any questions or concerns you may have.
WHO Growth charts can be downloaded from the Dieticians of Canada webpage and should be used throughout your child’s life until they reach the age of 19 years old. Growth charts are gender specific and record weight, head circumference and length. Paediatricians and family doctors will be familiar with using these charts and can give you guidance on whether your baby is meeting the right milestones during routine check ups after plotting your baby’s growth and development.

We expect you to be resting for the first week and therefore our postpartum visits are not scheduled. Your midwife will come to visit anytime on the day arranged, sometimes this is early morning and sometimes later in the evening.
Your midwife will visit you at home or at the hospital twice during the first week with phone call check ups planned. You will then come to the clinic at two and six weeks postpartum, with a phone check up planned for week four unless your midwife feels your baby needs to be seen in-person during this appointment.
If your midwife is sleeping from a birth, another midwife will be organized to visit you or your midwife may decide to reschedule for the next day if you and baby are stable.
Please do not page the on-call midwife about your home visits in case she is at a birth or sleeping. If it’s more convenient for you to come to the clinic for your early postpartum visits, this can be arranged instead of home postpartum visits.
Please ensure during the winter months your driveway is shovelled and gritted for the safety of our midwives. During times of a snowstorm or unsafe driving conditions, your midwife will contact you to make other arrangements.
All pets should be caged, or placed in another room during your midwife’s home visits. Due to health & safety as well as allergies and fear of animals, our midwives and their equipment cannot come into contact with your pets.
During the initial weeks after you have your baby you can refer to this online guide, our resources page as well as watching the educational videos in our postpartum section to assist you with any questions or concerns you may have.
WHO Growth charts can be downloaded from the Dieticians of Canada webpage and should be used throughout your child’s life until they reach the age of 19 years old. Growth charts are gender specific and record weight, head circumference and length. Paediatricians and family doctors will be familiar with using these charts and can give you guidance on whether your baby is meeting the right milestones during routine check ups after plotting your baby’s growth and development.


Perineum:
Applying ice pads, padsicles or chilled herbal bath compresses may help to ease discomfort.
Try urinating while using your cleansing bottle (or while in the shower or tub) if it is uncomfortable for the first day or two. You may find it helpful to support your perineum during a bowel movement (hold a clean cloth or compress to the area). It is important not to “hold in” a bowel movement – resting your feet on a low stool and relaxing your pelvic floor will also help.
Your discharge may smell “fleshy” but should not have a foul odour. The sanitary pads you purchase to use at this time should have a cottony surface. Do not use tampons and do not use pads that are a “dry weave” texture as they cause irritation and impede proper healing of the perineum.
What is normal in the first week after my baby is born?
Breasts:
About the third day after your baby is born, your milk will “come in” and your breasts will feel full. To relieve any discomfort, try massaging your breasts gently but do not express your milk (or you may make more), take a warm shower or use warm and cold compresses. Nursing your baby frequently is the best way to prevent discomfort. If you plan to formula feed or you are planning to suppress your milk supply, frozen cabbage leaves can be placed down your bra to dry up your milk supply and relieve discomfort.
If your breasts are hard and reddened, or so full that your baby is unable to latch properly, you may be experiencing engorgement. You can try expressing a small amount of milk until the nipple is softer to allow your baby to latch easier.
Your nipples may feel somewhat tender and sting when your baby first latches on while breastfeeding is getting established. They should not be painful throughout a feeding, and should not be blistered or cracked.
Apply a nipple ointment to relieve any discomfort after every feed. You are not required to wash this off before the next feed. If the nipples continue to be damaged, a prescription ointment can be prescribed by your midwife to assist with healing.
We have some educational videos that demonstrate good latching technique, positioning of your baby and other tips you may find useful.
If you have difficulties or challenges with breastfeeding, there are many groups offering assistance that you can attend. A public health nurse can also be another source of assistance and may organize a home visit. Private lactation consultants can be found using a google search, and can be helpful for extra support if you are struggling with your breastfeeding journey.
Bleeding:
You will experience red bleeding and may pass some small clots for about three days; your discharge will then turn brownish and mucousy and will continue for 10 days to 6 weeks. If your bleeding becomes heavy, we often advise you to first empty your bladder, as a full bladder can impede your uterus from contracting and slowing bleeding to a normal level. Should your bleeding continue to be heavy; filling two heavy pads within 30 minutes, someone “turned the tap on” or is a slow and steady trickle that is not relieved after urination, you should call 911 and return to the hospital.
Afterpains:
It is normal to have strong cramps or “afterpains” for a day or so after the birth, especially when the baby nurses. Clients having second or subsequent babies will notice them more than those having a first baby. Tylenol and Ibuprofen/or naproxen are safe to take while breastfeeding – ask your midwife about the dosage or follow instructions on the medication bottle.

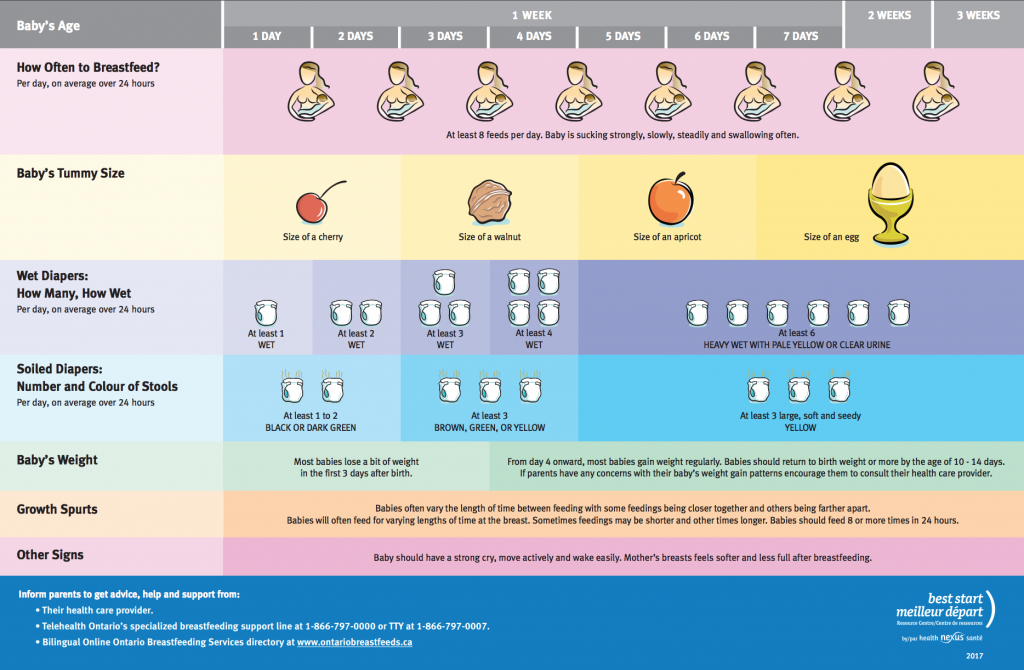
Feeding your baby:
Baby should be feeding at least every 3 hours on average in the first two weeks. Baby may be feeding as often as hourly at times. Each feed will take an average of 10-30 minutes. You should wake your baby to feed if it has been longer than 4 hours after your baby’s last feed. It is a good idea to drain one breast first, then offer baby the second. Note: it is okay if baby only feeds from one breast at a feeding. Many breastfed babies do not need extra burping. Breastfed babies do not need extra water, even in hot weather.
Emotions:
Temporary feelings of inadequacy and crying for no apparent reason are natural responses to hormonal changes and sleep deprivation – the so-called “baby blues” that happen in the first few days after the birth. If these feelings persist or worsen, or if you are feeling so low that you are unable to cope and care for the baby and yourself, contact your midwife for help immediately.
Registering your baby's birth:
Service Ontario offers an online birth registration option to allow you to register the birth, get a birth certificate, apply for a Social Insurance Number, and sign up for Canada (Ontario) child benefits.
Pee and Poop:
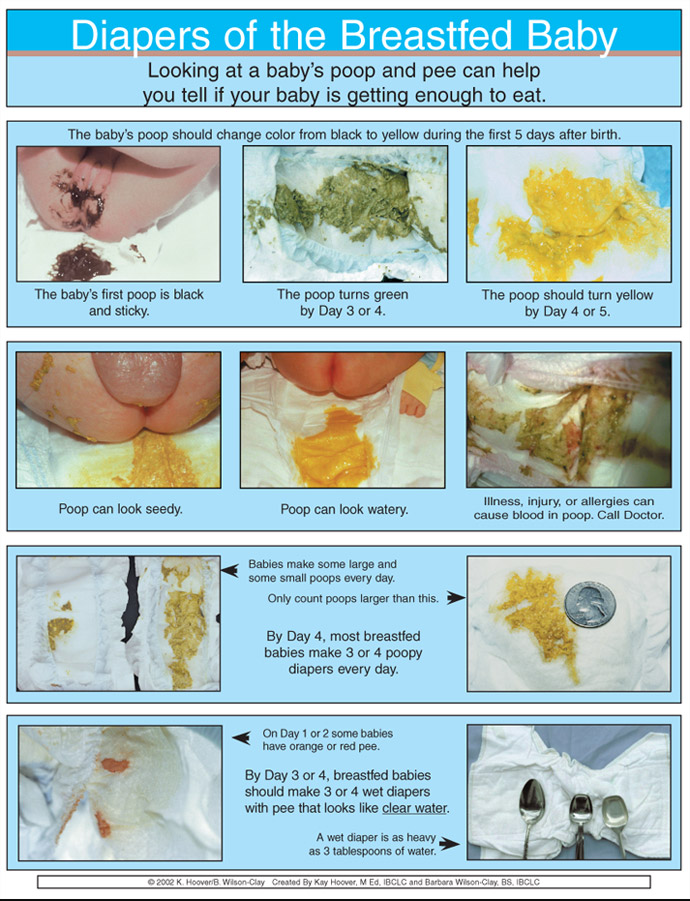
In the first few days of life before your breastmilk comes in, you may find an orange/red “brick dust” substance in baby’s diaper. This is uric acid crystals, and is more common in boys than girls. Some girl babies will have a pinkish or white mucous discharge in the first few days of life, and some will have a “mini period”. This is normal and should not be cleaned aggressively. Once your milk comes in, baby should have at least one or two bowel movements per day; one bowel movement per feeding is not uncommon. Once your milk comes in, baby should have 6 to 8 soaking wet diapers per day. If using disposables, you may want to place a tissue inside baby’s diaper in the first few days to help you check that it is wet.
Formula fed babies after they have passed the meconium over the first few days, have yellow, tan or brown poops that can be liquidy or solid but usually the consistency of peanut butter. They can also have more green poops if they experience too much iron in their diet which is normal as long as it is not accompanied by constipation i.e. baby has not pooped for 10-14 days. If you find your baby is constipated or there is blood in the stool, you should discuss switching formula brands with your paediatrician or family doctor to a brand without fortified iron.
It is normal for babies to go several days and up to 2 weeks without a bowel movement. Despite this being uncomfortable for your baby, you can try bicycling your baby’s legs to get the bowels moving especially if your baby has some trapped gas.
Cord Care:
Do not use alcohol to clean the cord stump; the cord does not require any special care and will only take longer to fall off if alcohol is used. Baby’s cord stump will usually fall off after 5 to 10 days. Try to keep the top of the baby’s diaper away from the stump. The stump may smell foul for a day or so before it falls off. The stump may look reddish and bleed a little bit which is normal, but if the skin surrounding the stump is red and swollen, contact your midwife.
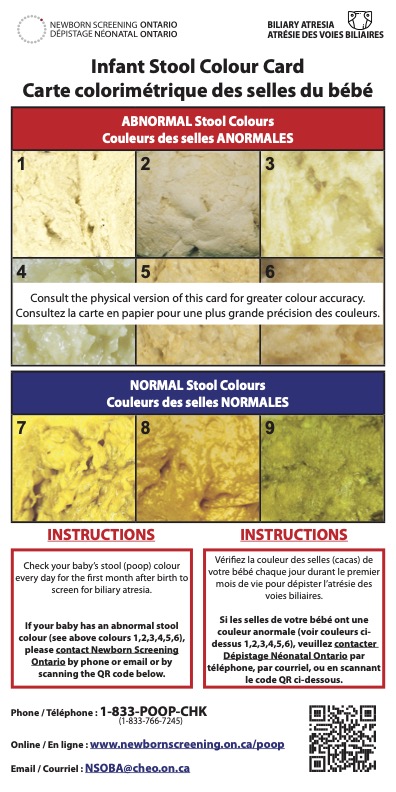
Biliary Atresia:
What is biliary atresia?
Biliary atresia (BA) is a rare but serious disease where bile cannot get from the liver to the stool (poop). Babies with BA usually seem well but they can develop pale yellow or whitish coloured stools in the first month of life. Along with the pale poop, these babies can have yellow skin and eyes (jaundice) lasting longer than the first two weeks of life. Without treatment, babies with BA will develop life-threatening liver damage. Treatment is most effective when babies are identified before they are one month old.
How can you screen for biliary atresia?
You can screen for BA by comparing your baby’s stool (poop) colour to the numbered pictures on the front of this card, for the first month after birth. Screening for abnormal stool colour can help to identify problems with the liver earlier. Keep this card close by when you change your baby’s diaper.
Who do I contact and when?
If at any time during the screening you notice that your baby has an abnormal stool colour (number 1,2,3,4,5, or 6), please contact your midwife or the Newborn Screening Ontario using the information on the front of this card. Please have available the baby’s name, birth date, and health card number.
What happens next?
First, don’t be alarmed. This is a screening tool and not a diagnostic test. A clinical team member from Newborn Screening Ontario will return your call by the next business day to discuss your concern and begin next steps. Your privacy and health information is protected.
For more information about biliary atresia, visit our website or scan the QR code on the front of the card.
Information is available in other languages. www.newbornscreening.on.ca/poopcard
Eyes:
Some babies get “sticky eyes” (some yellowish discharge). The eyes can be washed with a clean cloth or cotton ball using a saline solution equal to 1 tsp. salt to 2 cups of water (or 5 ml salt to a half litre of water). You may also squirt or drop some expressed breastmilk into baby’s eye. Call your midwife if the white of the eye is inflamed, if the discharge is green, or if it is spreading or worsening.
Breathing:
You may start to notice your baby will have a fairly irregular breathing pattern. Sometimes they breath hold briefly and sometimes they breathe really quickly for short bursts of time. These are all normal newborn breathing patterns.
You should contact your midwife immediately if you notice your baby is having difficulty breathing such as; grunting noises, flaring of the nostrils, and rapid breathing that continues with holding your baby and you can see your baby’s chest drawing inwards to the ribs. These can be signs of respiratory distress or infection. Call 911, if your baby stops breathing for more than 10 seconds.
Skin:
Baby normally has some “milia” that look like little whiteheads on the skin. They should be left alone and will go away in time. If the baby’s skin is very dry at the creases, apply coconut oil or a hypoallergenic lotion to the affected area(s). You can also make an all-natural baby lotion that smells delicious and soaks into your baby’s skin by following the recipe here.
Normal temperature – 36.5 deg C to 37.5 deg C. (97.8F to 99.5F). Temperature should be taken a couple of times under your baby’s armpit.
If your baby’s temperature is over 37.5, unbundle your baby, but do not undress completely (as your baby may get too cold) and retake your baby’s temperature in 30 minutes. Recheck your baby’s temperature again after these measures. If your baby temperature is over 37.5 and you have taken the above actions, you should contact your midwife.
Jaundice:
As explained above, jaundice is the yellow colour of your baby’s skin caused by a pigment known as bilirubin, which is broken down by the liver to remove the pigment from the blood. Feeding your baby often (especially breastfeeding) in the first week can help to break down the bilirubin pigment faster because the more your baby can pee and poop, the faster the jaundice can be expelled.
Mild to moderate jaundice is not harmful to your baby. However, large amounts of bilirubin in your baby’s blood can cause a condition called kernicterus, which can lead to brain damage. To prevent this from happening, your midwives will closely monitor your baby for “too much” jaundice and send your baby for a blood test if too much jaundice is suspected.
Jaundice can last for a two to three weeks and sometimes turn into “breastmilk jaundice” which is harmless and can last longer.
You should contact your midwife immediately if your baby’s skin becomes extremely yellow or the jaundice becomes worse, your baby is very sleepy or hard to wake, your baby is refusing to feed, and/or your baby has fewer wet diapers or bowel movements than expected from the chart above according to age.

The baby in the photograph has too much jaundice and has been placed under special blue lights called phototherapy to help the liver break down the bilirubin faster to safe levels where jaundice will not cause harm.

Safe Sleeping:
Here are a few links for sleep safety:
Baby should be placed on it’s back in the crib or bassinet, with no pillows, bumper pads, stuffed toys, or positional devices that could be a potential suffocation hazard, either swaddled or in a sleep sack to prevent Sudden Infant Death Syndrome (SIDS). Do not over bundle your baby. Place your baby to sleep in a crib, cradle or bassinet next to your bed.
Baby car seats, swings, and bouncers are not safe substitutes to a crib or bassinet. Soft bedding, such as pillows, comforters, quilts, other soft surfaces such as adult beds, sofas and armchairs, can increase the risk of suffocation.
Ever heard the term “Don’t wake a sleeping baby”…well that does not apply to car seats or other carrying devices. A car seat should only be used for when you are traveling. A recent report by the Journal of Paediatrics, identified 47 deaths of children under the age of 2 over a 4 year period. The deaths occurred while children were placed in the car seat outside of a car (31 deaths) or other carrying device (bouncer, stroller). Parents often think car seats are one of the safest places for baby to nap. However, when your baby is in the car, the base is levelled at an angle, which keeps your child’s airway open. When your car seat is out of the car, your baby is more likely to slouch forward, causing a condition called positional asphyxia, cutting off your child’s oxygen supply. Positional asphyxia can also happen in a bouncy chair, swing or other device. If your child is not repositioned quickly enough, it can lead to brain damage and eventually death. Most, if not all, of these deaths could have been prevented by moving baby into the crib.
Reminder:
Place your baby on their tummy 2-3 times a day soon after your baby is born. Slowly work your way up from 1 minute of tummy time, each time, until your baby can hold up their head, often around 3-4 months.
As babies get older they are usually able to turn over onto their tummies by themselves, often around 5 months. When this happens you do not need to reposition your baby onto their back to sleep.
Group B Strep:
You can read about Group B Strep (GBS) here.
After your baby is born, your midwives will monitor your baby for signs of GBS infections. Early-onset GBS can occur between 6 and 7 days of age, and cause infections in the lungs, brain, spinal cord and blood. This is the infection that the antibiotic treatment in labour helps to prevent 90% of the time.
Late onset GBS is a second type of GBS disease occurring 7 days after the birth up to several months later and is not always related to the birth process. There is currently no way to prevent GBS disease but knowing the signs and when to seek medical attention is important.
We advise you to ensure your family and friends wash their hands before touching your baby, as GBS could potentially be transmitted from person-to-person.
Signs of GBS:
- Blue appearance (cyanosis)
- Breathing difficulties – grunting, flaring of the nostrils, rapid breathing, short periods without breathing
- Lethargy (baby very tired)
- Pale appearance (pallor) with cold skin
- Poor feeding
- Unstable body temperature (low or high)
Vitamin D for baby:
You can read more about starting vitamin D for the baby here.
If your are breastfeeding, we recommend you begin giving your baby 400IU of vitamin D per day starting in the first week after birth until your child is no longer breastfeeding. Formula fed babies do not require vitamin D supplements as formula contains vitamin D.
Car Seat Safety:
Click here for the latest updates in car seat safety, installing your car seat, how to buckle your baby into the car seat properly, choosing the right car seat as your child grows – currently you will choose Stage 1 rear facing seats. Click here for choosing the right car seat according to weight and height.
Returning to "Normal"
Exercise:
Many clients want to know when they can return to their daily lives, specifically exercise. We recommend commencing kegels exercises shortly after birth, whether you had a vaginal or a caesarean section.
Healthy lifestyle guide:
You can read or review other aspects of leading a healthy lifestyle in the postpartum including nutrition, supplements, healthy gut, specific diets like vegetarian, vegan, dairy free, or gluten free diet, alcohol and breastfeeding, smoking, and marijuana use.
Clients also want to know when they can get back to the gym, get back to volleyball or soccer games, begin to get out for a run, etc. Well this answer is not so simple. It really does depend on the type of delivery you have had, whether you have had stitches, how well things are healing, etc. We do recommend that you take it easy for the first six weeks. You can read more below and follow up with your midwife for recommendations.
Educational videos and resources:
We have many educational videos in our postpartum section including; what your midwife will do in the postpartum, circumcision, bathing your baby, swaddling your baby, soothing your crying baby, diapering and dressing your baby, breastfeeding demonstrations, how to make a formula bottle, sterilizing your equipment, burping your baby, skin to skin, and delayed cord clamping.
Life after you leave your midwife:
Family doctor or paediatric care:
It is your choice which care provider you wish to continue using after your final discharge appointment with your midwife.
Clients can choose to continue with their family doctor, or they can begin searching for a paediatrician (baby doctor) after the birth. Some paediatricians will be full, so we recommend calling around to find someone that is currently accepting babies.
Your midwife will need the name of your chosen care provider to send a discharge letter after your 6 week visit.
Vaccinations:
Vaccination schedules begin once your baby reaches 8 weeks old. Your baby will be under the care of their new doctor at this point, so you can read more about deciding to vaccinate, how vaccinations work, when to vaccinate, vaccine effectiveness, diseases that vaccinations prevent and what to expect at the vaccination appointment at the following link:
References:
- La Leche League Canada – skin-to-skin contact
- Canadian Breastfeeding Foundation – The importance of skin-to-skin contact.
- Canadian Paediatric Society – Vitamin K prophylaxis in newborns
- Association of Ontario Midwives – Eye prophylaxis position statement
- Canadian Paediatric Society – Preventing ophthalmia neonatorum
- Canadian Paediatric Society – Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants
- Canadian Paediatric Society caring for kids – Jaundice in newborns
- Ontario Hearing screen
- Ontario Newborn Screening
